Sleep Apnea (OSA)
How Common is OSA ?
Obstructive Sleep Apnea (OSA) is the second most common sleep disorder in the World (Insomnia is the first). The World Health Organization (WHO) recognizes OSA as a “Growing epidemic.”
Over 1 billion people in the world have OSA. In the United States it is estimated that 80 Million Americans have OSA; approximately 50% are undiagnosed.
Ninety-four percent (94%) of individuals with OSA have Snoring as a symptom!
In the United States, approximately 8 million individuals are placed on CPAP masks each year for OSA – but 30-50% QUIT or don’t fill their prescription within the First Year. Accordingly, there are approximately 4 million NEW CASES of UNTREATED Sleep Apnea per Year – Every Year!
UNTREATED Sleep Apnea has Devastating and has Lethal consequences.
These are just a few:
- 200% ↑ Risk Heart Attack
- 200% ↑ Risk Stroke
- 300% ↑ Risk Death
There is GREAT financial incentive to place patients on the CPAP mask – even if the results of CPAP treatment are inconsistent. For instance, reports note that “…the global CPAP devices market size was evaluated at 2.41 Billion USD in 2020, which has grown by over 4.2 Billion by 2022”… and is expected to Continue to Grow! The WHO considers sleep apnea an “expanding epidemic.”
The diagnosis of OSA has increased 442% from 1999 to 2010 according to the National Ambulatory Medical Care Study. From 2019 to 2022 there has been approximately a 180% increase in OSA in the United States.
Common Symptoms OSA
There are many signs of Sleep Apnea – many are quite obvious.
They include the following:
- Loud Snoring (94%)
- Breathing through Mouth while asleep
- Waking – Gasping for air during sleep
- Waking w Sore throat / Hoarse Voice
- Waking w Headaches
- Wake up Not feeling rested
- Waking w Dry Mouth
- Frequent Waking
- Headaches During Day
- Daytime Sleepiness – Fatigue – Napping
- Difficulty w Cognition – Concentrating
- Memory Loss
- Anxiety / Depression
- Changes in Mood – Behavior
- Urinary Urgency
- Urinary Frequency
- Incontinence
- Nocturia
- Increase in Car accidents and accidents at work
- Compromised work performance
- Poorer general health
We utilize numerous Patient Questionnaires to detect cases of underlying sleep apnea.
Associated Illnesses (Comorbidities) of OSA
There are many associated illness with Sleep Apnea; these are called “comorbidities” which frequently are found in patients who have OSA. Many of the patients with the following medical conditions also have OSA. Those medical conditions range from Metabolic Disorders, Neuropsychiatric Disorders, and even malignant neoplasms.
They include the following:
- Associated General Metabolic Disorders
- Acute Myocardial Infarction
- Hypertension
- CHF – Congestive Heart Failure
- CVA – Stroke
- Atherosclerosis – Endothelial Damage – Ischemia
- Cardiac Tachyarrhythmias (Atrial Fibrillation; etc.)
- COPD – Emphysema
- Depression
- Dementia – Alzheimer’s
- CRF – Chronic Renal Failure
- Peripheral Neuropathy
- Metabolic Syndrome
- Obesity
- DM: Diabetes Mellitus
- IBS: Inflammatory Bowel Disease
- Non-Alcoholic Fatty Liver Disease
- Associated Neuropsychiatric Disorders
- Depression
- Irritability
- Decreased attention Span
- Loss of Short Term Memory
- Associated Malignant Neoplasms
- CNS Neoplasms
- Lung Cancer
- Melanoma
- Breast Cancer
- Colorectal Cancer
- Pancreatic Cancer
- Prostate Cancer
- Urinary Cancer
- Uterus Cancer
Bidirectionality of Comorbidities
An often overlooked feature of OSA is the growing substantial evidence of its “Bidirectionality of Comorbidities.” Overlooking this feature of OSA makes it nearly impossible to effectively treat OSA.
The Bidirectionality of Comorbidities represents the axiom that not only is OSA associated with various illnesses or co-morbidities as listed above, but that OSA is an Independent Risk Factor for the Development of these Comorbidities – and that – some Comorbidities may Predispose To the Development of OSA.
Just as an example, there is substantial scientific evidence to indicate that OSA is not only associated with hypertension (high blood pressure), but hypertension, itself, is an independent pre-disposing factor to the development of OSA.
Treating only one side of this equation of bilaterality, is scientifically – and Clinically – unintelligible and meaningless.

What Happens During Sleep Apnea – Why is Untreated Sleep Apnea So Deadly ?
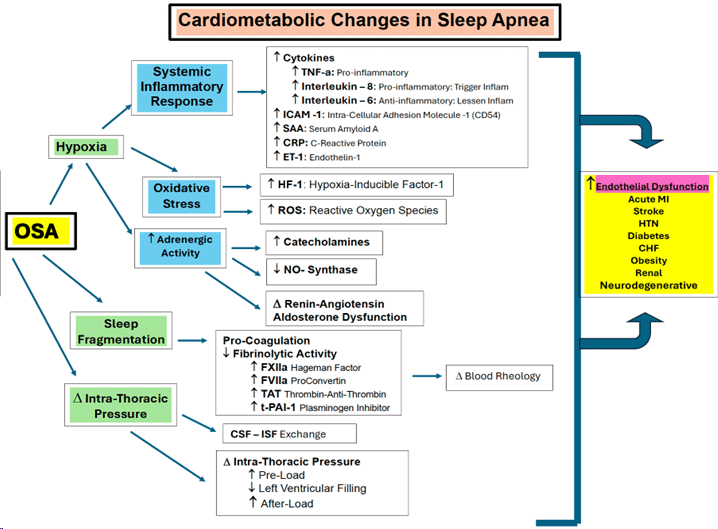
There a LARGE number of cardiometabolic, neurometabolic and neurohumoral changes which occur during sleep apnea – BECAUSE – your body is NOT RECEIVING OXYGEN for PROLONGED PERIODS of time. That is NOT conducive with life.
As the diagram shows, it all begins with three (3) devastating features of sleep apnea:
-
- Hypoxia
- Sleep Fragmentation
- Changes in Intra-Thoracic (Chest) Pressure
Each of these initiating features is followed by enormous consequences.
Hypoxia: Hypoxia sets off a particularly devastating cascade of:
-
-
- Systemic Inflammatory Response: this response is heralded by a massive increase in Pro-inflammatory Cytokines and other proteins which lead to enormous endothelia destruction (deterioration of the inside lining of your blood vessels). Endothelial destruction compounds the possibility of blood clot formation which often lead to acute myocardial infarction (heart attack), cerebrovascular accidents (CVAs; Stroke), pulmonary emoboli (blood clots to the lung), etc.
- Oxidative Stress: Our internal biologic systems include literally millions of chemical reactions occurring simultaneously. They occur in concert so as to maintain a proper chemical and metabolic “balance” or “homeostasis” within all parts of our body.
When hypoxic conditions occur, as in Sleep Apnea, there is a rapid proliferation and activation of Pro-inflammatory cytokines which require our bodies to markedly increase our internal metabolism in order to maintain energy homeostasis. This rapid increase in metabolism causes a rapid increase metabolic byproducts – called Free Radicals. Now, the balance becomes “broken.”
The free radicals are collectively commonly referred to as Reactive Oxygen Species (ROS). ROS include chemical byproducts like superoxide radicals, hydrogen peroxide, hydroxyl radicals, and singlet oxygen – they are all Unstable. These byproducts are “unstable” because they lack the necessary number of electrons to be “stable.” These free radicals “search” for electrons they can steal from other molecules in our bodies to regain their stability – thereby damaging other cells and putting them at risk of instability.
To avoid the imbalance from causing havoc in our bodies, our physiologic systems include “Anti-Oxidants.” Our naturally occurring internal physiologic anti-oxidants include Vitamin A, Vitamin C, Vitamin E, Copper, Zinc and Selenium.
Thus, there is a “balance” between the Anti-Oxidants in our system and the Pro-inflammatory cytokines. When that balance is outweighed by metabolic free radicals such as ROS, the condition of Oxidative Stress results.
Scientific evidence has shown that oxidative stress and inflammation are the root cause of over 260 diseases.
- Increased Adrenergic Activity: The disordered breathing of Sleep Apnea causes dysregulation of the autonomic cardiovascular system. Hypoxia (LOW OXYGEN) and hypercapnia (HIGH CO2) cause an INCREASE in the activity of the sympathetic nervous system.
Normal sleep is a time of low physiological strain. This is evident through the non-rapid eye movement (NREM) phase of sleep where sympathetic nervous (stimulating) activity DECREASES and parasympathetic (quieting) activity INCREASES. Thus, normal sleep is associated with a decreased muscle sympathetic nerve activity resulting in natural decreases in Blood Pressure (BP) and Heart Rate while in deep NREM sleep as compared to being awake.
In contrast, patients with Sleep Apnea, BP and sympathetic nerve activity do NOT fall during sleep. Intermittent apnea, hypoxemia and hypercapnia result in SIGNIFICANT INCREASES in sympathetic nervous system outflow. This often results in vasoconstriction-induced surges in BP to extreme levels. This type of Increase in neural adrenergic sympathetic activity leads to cardiovascular variability is a key marker of Increased cardiovascular risk.
-
Sleep Fragmentation: Sleep fragmentation initiates pro-coagulation processes which increase the chance of blood clot formation and decrease the likelihood that your body will be able to dissolve any blood clot which may be formed. These blood clots can lead to acute myocardial infarction (heart attack), cerebrovascular accidents (CVAs; Stroke), pulmonary emoboli (blood clots to the lung), etc.
Changes in Intra-Thoracic (Chest) Pressure: When you stop breathing during sleep apnea, the pressure within your chest changes as a result of your lungs not moving air; your chest movement essentially comes to a stop. As a result, blood flow into your cardiac chambers, which is ONLY facilitated by changes in pressure (because your heart is NOT a “pump” contrary to public opinion).
These changes in chest pressure and blood flow cause stagnation of blood on the right side of your heart (Increased Pre-Load), Decrease in filling of the left side of your heart (thus, Decreased cardiac output), and Increase in the Pressure (Resistance) on the left side of your heart which your heart faces when trying to deliver blood from the heart to all parts of your body (Increased Afterload).
The result: MARKEDLY Increased Cardiac Strain and Ischemia on your heart – leading to Heart Attack and Cardiac Arrythmias. In fact, the Most Common Cause of Death from Sleep Apnea is Cardiac Arrythmias (either atrial tachyarrhythmias or ventricular tachyarrhythmias (most commonly Atrial Fibrillation).
How is Sleep Apnea Diagnosed ?
In general, to determine whether you have Sleep Apnea, a number of steps are undertaken:
- Pre-Screening Questionnaires – these sets of Questionnaires are important for Patients to complete to determine whether Snoring exists, the extent of Snoring, and to determine whether there are any underlying Sleep Apnea issues which the Patient may or may not be aware of:
- General Health Questionnaire
- Thornton Snoring Questionnaire
- Epworth Sleepiness Questionnaire
- Nasal Obstruction Questionnaire
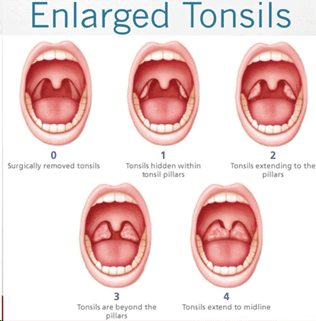
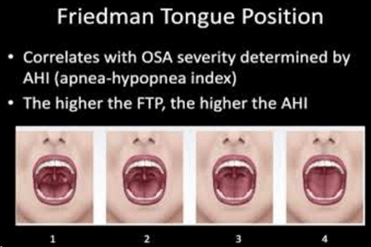
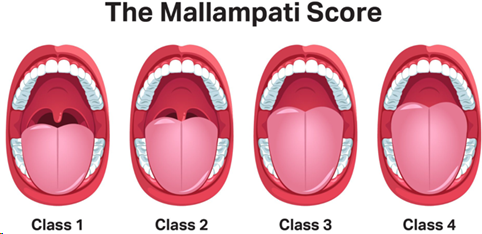
- Brief Physical Examination – Examination of the oral cavity is very important in the evaluation of snoring and sleep apnea. The relationship of the tongue and the opening or size of the posterior pharynx is evaluated for degrees of potential airway obstruction. Examination of the Tonsils, Tongue, and Mallampati Score (an assessment of the relative size of the base of the tongue compared to the oropharyngeal opening in determining and predicting a difficult and compromised airway) are key considerations.
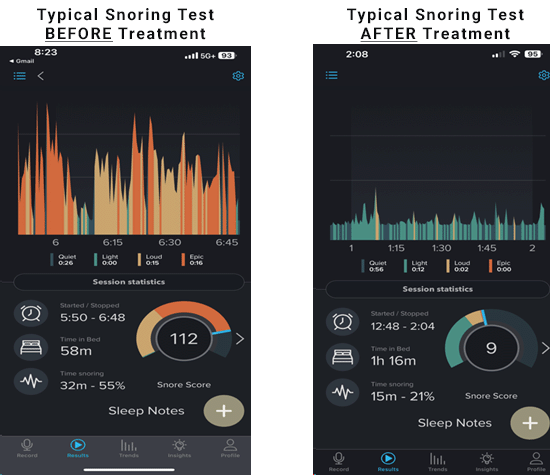
- Snoring Verification (cell phone app)
This is an example of the remarkable type of improvement we expect after NightLase® Laser Therapy for snoring. This is an example of a cell phone app which measures the degree of snoring Before and After NightLase® Laser Therapy.
- Sleep Apnea Test – this the main diagnostic tool which a clinician relies upon to diagnose and manage Sleep Apnea. It is a test which can be performed with a simple finger attachment used while the patient sleeps at their own home, or, it can be performed in a facility which has a “sleep lab.” Modernly, the technology of outpatient finger-sleep apnea testing is highly advanced, inexpensive, and reliable. The key determinant of a Sleep Apnea Test is the “Apnea – Hypopnea Indes” or “AHI.” This determination delineates how many episodes of Apnea and Hypopnea a individual has, per Hour, during a night sleep.Apnea: Number of apneas:
An apnea is a total or near total lapse in breathing, indicated by STOPPING Breathing or a Reduction in airflow of 90% for at least 10 seconds.Hypopnea: Number of hypopneas:
A hypopnea is a partial reduction in breathing for at least 10 seconds and involves at least a 30% drop in airflow.
As an example, if an individual has an AHI score which indicates 16 episodes of Apnea – that means that in one hour (60 minutes) the individual either STOPPED Breathing or had a Reduction in airflow of 90% for at least 10 seconds 16 times per hour (about every 3 minutes!)
