Understanding the Risks
The Severe Impact of Snoring
Discover how snoring can lead to serious health issues and learn about effective treatments to mitigate these risks.
Many individuals, and their partners, suffer from “Snoring.” Snoring interrupts the peace and tranquility of sleeping (for everyone concerned) and is a form of what is called “Sleep Disordered Breathing” (SDB).
Snoring is actually the “sound” of “obstructed breathing.”
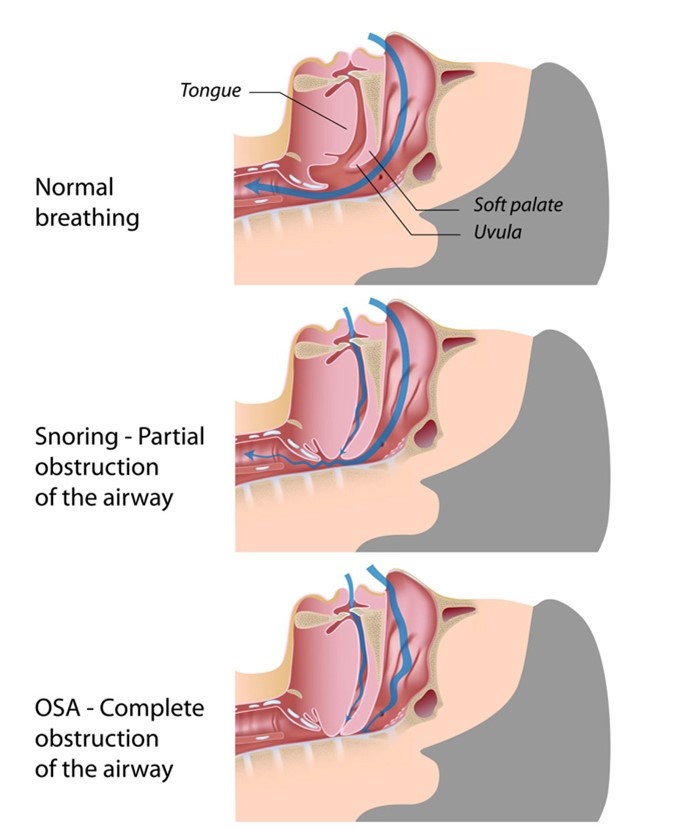
Obstructed breathing can result from abnormal structures in the back of your throat. That includes poor muscle tone, bulky throat tissue, a long soft palate, or a long uvula.
The “uvula” is that part of the fleshy extension of the back of your soft palate which you can easily visualize when your mouth is wide open which hangs above the throat. It looks like a “punching bag” hanging in the back of your throat. It is made of connective tissue and small muscle fibers and secretes saliva to keep your throat well lubricated.
As illustrated, at night, when you are trying to sleep, your tongue and pharyngeal muscles may fall backwards due to size and poor muscle tone, consequently causing a Partial obstruction – that causes Snoring.
When there is Complete obstruction, Sleep Apnea results.
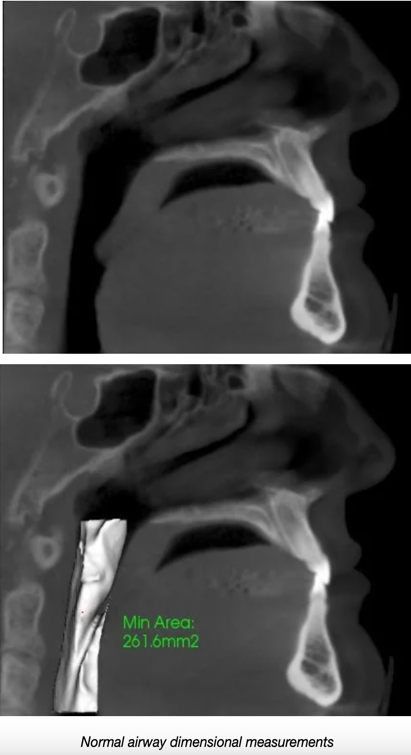
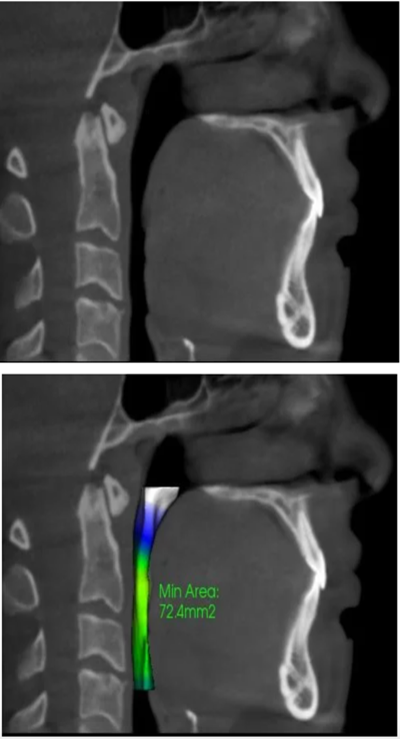
These are examples of normal and restricted airway volumes due to airway obstruction:
Do you have a larger image?
Sleep Apnea occurs when there are periods of either “Apnea” or “Hypopnea” – usually Both.
Apnea consists of a period of time when you actually STOP BREATHING and your brain, heart and entire body receive NO OXYGEN. If you stop breathing – or – have a 90% Drop in airflow for 10 seconds, it will be recorded in the Sleep Apnea Test as an “apneic” period.
Hypopnea consists of a partial reduction in breathing for a 10 second period of time and involves at least a 30% drop in airflow.
Metabolic Effects and Risks of Simple Snoring
Simple snoring – that is Snoring not associated with Sleep Apnea – ALSO has SEVERE and SERIOUS metabolic effects and risks.
For instance: SNORING Increases:
(1). Obesity
(2). High Blood Pressure
(3). Heart Attack
(4). Diabetes
(5). Metabolic Syndrome
(6). Triglyceride Levels
(7). Death Rate
- Zou J, Song F, Xu H, Fu Y, Xia Y, Qian Y, Zou J, Liu S, Fang F, Meng L, Yi H, Guan J, Zhu H, Chen B, Yin S. The Relationship between Simple Snoring and Metabolic Syndrome: A Cross-Sectional Study. J Diabetes Res. 2019 Apr 10;2019:9578391. doi: 10.1155/2019/9578391. PMID: 31093507; PMCID: PMC6481037.
- Rich J, Raviv A, Raviv N, Brietzke SE. An epidemiologic study of snoring and all-cause mortality. Otolaryngol Head Neck Surg. 2011 Aug;145(2):341-6. doi: 10.1177/0194599811402475. PMID: 21493281.
- Xiong X, Zhong A, Xu H, Wang C. Association between Self-Reported Habitual Snoring and Diabetes Mellitus: A Systemic Review and Meta-Analysis. J Diabetes Res. 2016;2016:1958981. doi: 10.1155/2016/1958981. Epub 2016 Jan 19. PMID: 26904689; PMCID: PMC4745979.
- Koskenvuo M, Kaprio J, Partinen M, Langinvainio H, Sarna S, Heikkila K. Snoring as a risk factor for hypertension and angina pectoris. Lancet. 1985;1:893–6.
- Koskenvuo M, Kaprio J, Telakivi T, Partinen M, Heikkila K, Sarna S. Snoring as a risk factor for ischaemic heart disease and stroke in men. Br Med J (Clin Res Ed) 1987;294:16–9.
- Hu FB, Willett WC, Manson JE, et al. Snoring and risk of cardiovascular disease in women. J Am Coll Cardiol. 2000;35:308–13.
- D’Alessandro R, Magelli C, Gamberini G, et al. Snoring every night as a risk factor for myocardial infarction: a case-control study. BMJ. 1990;300:1557–8.
- Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41.
- Mooe T, Franklin KA, Holmstrom K, Rabben T, Wiklund U. Sleep-disordered breathing and coronary artery disease: long-term prognosis. Am J Respir Crit Care Med. 2001;164:1910–3
- Zamarron C, Gude F, Otero Otero Y, Rodriguez-Suarez JR. Snoring and myocardial infarction: a 4-year follow-up study. Respir Med. 1999;93:108–12.
- Lindberg E, Janson C, Svardsudd K, Gislason T, Hetta J, Boman G. Increased mortality among sleepy snorers: a prospective population based study. Thorax. 1998;53:631–7.

